.png)
Panic Diary: A Tracking Tool for Understanding Anxiety Patterns
Short Description

Content Details:
The Panic Diary is a therapeutic tracking worksheet designed to help clients move from experiencing panic as overwhelming and unpredictable to understanding it as a pattern they can learn to manage. By documenting the details of each panic episode, clients build awareness of their unique triggers, physical symptoms, and coping responses, creating a foundation for more effective intervention.
This resource is ideal for clients working through panic disorder, generalized anxiety disorder, or situational anxiety. It pairs well with CBT, DBT, exposure therapy, and other evidence-based modalities that emphasize self-monitoring and insight development.
What makes this tool effective:
Panic attacks often feel like they come out of nowhere, which reinforces the fear cycle. The Panic Diary interrupts that narrative by helping clients see connections they might otherwise miss, whether it's a time of day pattern, a physical sensation that precedes full panic, or environmental factors that increase vulnerability.
The structured format reduces cognitive load during high-stress moments. Clients don't have to figure out what to track or how to organize their thoughts. They just fill in the prompts. Over time, the diary becomes a personalized data set that both client and therapist can review to identify patterns, test hypotheses, and measure progress.
How to use this worksheet:
Print multiple copies or save as a reusable digital template. Encourage clients to complete an entry as soon as possible after a panic episode, ideally within the same day while details are still fresh.
Walk through the first entry together in session so clients understand what level of detail is helpful. Some may want to write paragraphs; others will benefit from brief notes. Both approaches work as long as they're capturing the key data points.
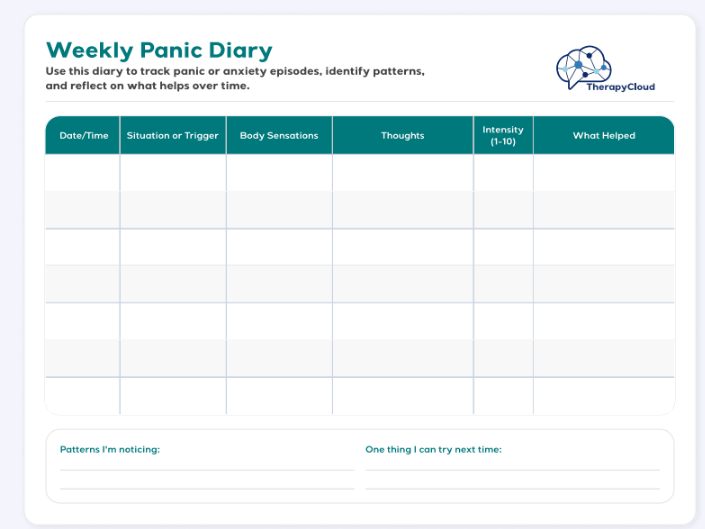
What to track in each entry:
- Date, time, and location when panic started
- What was happening right before (thoughts, activities, conversations)
- Physical symptoms experienced
- Intensity rating (typically 1-10 scale)
- What coping strategies were attempted and whether they helped
- How long the episode lasted
- Additional context (sleep quality, caffeine intake, stress levels, skipped meals)
Reviewing entries for patterns:
After collecting 5-10 entries, start pattern analysis. This is where raw data becomes actionable insight.
- Temporal patterns: Do panic episodes cluster around specific times of day? Many clients experience increased vulnerability in the morning (cortisol peaks) or late afternoon (blood sugar drops). Weekend vs. weekday patterns can reveal stress-related triggers.
- Physiological precursors: What physical sensations show up before full panic? Some clients consistently report stomach discomfort, muscle tension, or dizziness 10-15 minutes before a panic attack escalates. Identifying these early warning signs creates intervention windows.
- Cognitive triggers: Review the "what was I thinking" entries. Common thought patterns include catastrophic predictions ("something terrible is about to happen"), health anxiety ("I'm having a heart attack"), or loss of control fears ("I'm going to lose it in public"). When the same thought pattern appears repeatedly, you've found a cognitive target for intervention.
- Environmental factors: Look beyond the immediate trigger. Are there lifestyle patterns that increase vulnerability? Skipped meals, poor sleep, high caffeine intake, and accumulated stress often appear in the 12-24 hours before panic episodes. These aren't direct causes, but they lower the threshold.
- Avoidance patterns: If multiple entries involve similar situations (driving, crowds, specific locations), avoidance may be developing or already established. This is critical information for treatment planning because exposure work becomes necessary.
- Coping effectiveness: Which strategies actually helped? Clients often believe nothing works, but the data frequently shows otherwise. When deep breathing reduced intensity from an 8 to a 5, that's evidence worth highlighting. Pattern tracking reveals which tools deserve more practice.
- False alarms vs. cued panic: Some panic episodes have clear triggers (cued). Others seem to come from nowhere (uncued/spontaneous). The ratio matters for diagnosis and treatment approach. If most episodes are cued, exposure and cognitive work around those specific triggers will be most effective. If most are uncued, interoceptive exposure (deliberately inducing physical sensations) becomes more relevant.
- Recovery time: Track how long it takes to return to baseline after each episode. If recovery time is decreasing over weeks, that's progress even if panic frequency hasn't changed yet. It means the fear-of-fear cycle is weakening.
Key indicators of progress:
The diary transforms "I panic all the time" into "I panic most often on Tuesday mornings after poor sleep, usually triggered by thoughts about work performance." That specificity makes treatment significantly more targeted. Look for increasing pattern recognition, faster identification of early warning signs, more effective use of coping strategies, and clients' growing confidence that panic episodes are survivable and temporary.
What's included:
- Date and time fields
- Trigger identification section
- Physical symptoms checklist
- Emotional state tracking
- Coping strategies used section
- Duration and intensity rating
- Notes section for additional context
- Instructions for effective tracking and pattern analysis
This is a working document, not a perfection exercise. Some entries will be messy or incomplete, and that's fine. The goal is consistent tracking, not polished documentation. Every entry is useful information.